Tracheobronchomalacia (TBM) Program
About Our TBM Services
BIDMC offers advanced expertise in diagnosis and treating TBM, an under-diagnosed airway condition that causes chronic cough and infections.
BIDMC is a world leader in diagnosing and treating tracheobronchomalacia (TBM). If you've been diagnosed with TBM, you will benefit from our TBM Program which offers expertise from a multidisciplinary team of interventional pulmonologists, thoracic surgeons, ear/nose/throat specialists, speech pathologists, endocrinologists, general pulmonologists, behavioral health providers, anesthesiologists, and radiologists.
We evaluate and treat more patients with TBM than anywhere else in the United States. Through our TBM Program, we offer you an extraordinary level of expertise and care.
Normally the central airways (the trachea and bronchi) remain open when you breathe. In TBM, the airways become weak and floppy, tending to collapse with breathing.
TBM is a rare condition, and often misdiagnosed. In most cases, it is not clear what causes TBM. Sometimes it can be seen at the same time as another lung disorder, such as COPD, asthma, or cystic fibrosis. Our researchers are working to understand the underlying processes that lead to TBM. The treatment option that is right for you depends on how severe your condition is.
The sound of a cough before TBM treatment:
The sound of a cough after TBM treatment:
Other lung conditions, such as asthma, COPD, or emphysema, can cause symptoms that are similar to TBM. To ensure an accurate diagnosis, we offer patients one-stop access to a multidisciplinary team of experts.
Our specialists will first ask about your symptoms and past health problems, and do a thorough physical exam. They may also ask you to undergo two specialized medical tests — a dynamic flexible bronchoscopy and a dynamic expiratory CT scan — to determine whether you have TBM — and if so, how severe it is.
Dynamic Expiratory CT Scan
During a Computed Tomography (CT) scan, you lie very still on a table while multiple x-rays are taken of your throat and upper chest. A computer assembles these images to provide a detailed view of your airways.
To confirm or rule out a diagnosis of TBM, we conduct a dynamic expiratory CT scan. This means the CT scan will capture images of your airways as you breathe.
Dynamic Flexible Bronchoscopy
A bronchoscope is a long, thin, flexible tube that enables a doctor to look into your airways. This is the gold standard for diagnosing TBM because it permits real-time examination of the airways while you breathe. It also provides information on the extent and location of airway collapse.
We determine whether you have TBM, and how severe it is, by assessing your symptoms and how much your airway narrows when you breathe. If your TBM is diagnosed as mild or moderate, treatment is symptomatic and options include:
Airway Oscillatory Devices (Flutter Valve)
These are hand-held devices to help clear your airways. You inhale, and then exhale forcefully. This helps clear phlegm and mucus.
External Percussion Vests
These inflatable vests are connected to a compressor and help clear the lungs of mucus and phlegm. These are usually used 2 or 3 times a day.
Expectorant
This is a medication that makes it easier to cough up mucus and phlegm, clearing the airways.
Pulmonary Rehabilitation
This involves education and training to improve your quality of life. You will learn more about TBM, and how to breathe more productively, conserve energy, and keep active.
Pursed Lip Breathing
This is a breathing technique in which you inhale through your nose, while keeping your lips closed, and then exhale through tightly pursed lips. It is a simple yet effective way to slow your breathing and alleviate shortness of breath.
CPAP or BiPap Devices
A continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPap) device is used while you sleep. Both devices increase the air pressure in your throat, so that your airway doesn't collapse when you breathe.
If your TBM is severe, we conduct further tests to determine if you might benefit from a surgical procedure called tracheobronchoplasty. This procedure offers effective and permanent treatment for TBM.
To ensure that you will benefit from surgery, our multidisciplinary team will first determine whether you have other conditions that commonly occur in addition to TBM and need to be treated. For this reason, we will assess:
- Your vocal cord health
- Whether you have GERD (gastroesophageal reflux disease)
- Whether you have other lung disorders (asthma, COPD, emphysema)
We also determine whether you are healthy enough to undergo surgery.
Stent Trial
The final step in determining whether you will benefit from surgery is a 1-2 week "stent trial." The stent will keep your airways open, much as a cardiac stent keeps blood vessels open. This mimics what happens to your airways after surgery, so it will give you some idea of how much your symptoms will improve after surgery.
During the stent trial, using validated questionnaires (to assess shortness of breath, quality of life, and cough) we will monitor how you are doing and ask that you return to the TBM clinic for follow-up. In addition, you will undergo physiological evaluation using tests to assess lung function and 6-minute walking capacity. When the trial is over, we remove the stent. (We prefer not to implant stents permanently, as they can cause irritation or become infected. Surgery offers a better long-term solution for most patients.)
Tracheobronchoplasty
If your symptoms improve during the stent trial, and your overall health suggests you may benefit from surgery, we will schedule you for tracheobronchoplasty. Depending on your specific case, we have two possible approaches. The robotic-assisted approach consists of small incisions in the chest wall in which instruments are inserted to assist in repairing the affected area. The second approach is the open approach, which consists of a standard posterolateral thoracotomy incision and the surgeon opens the chest wall to reach the airways. In both methods, the surgeon sutures sections of mesh at multiple points on the outside of the floppy airway, to stabilize it (much like a splint will keep a broken bone steady). As you heal, scar tissue forms around the mesh, making it stable.
You will spend several days in the Intensive Care Unit, followed by a longer stay in the hospital. After you are discharged, we will monitor your recovery closely. Patients from out of state may need to find temporary housing in the area for the first month after discharge.
Post-Surgery Monitoring
We want to ensure that you recover as well as possible. For that reason, we ask that you return three months after surgery for evaluation. From then on, we will ask you to return to the TBM clinic once a year, so that we can continue to monitor your recovery.
Before Surgery
What testing is done before surgery and why?
Your doctor will perform many tests before considering surgery. We need to determine if your tracheobronchomalacia (TBM) is severe — are the windpipes very significantly collapsing? We typically do not treat mild forms of TBM because some collapse of the airway is actually normal and may not lead to symptoms. Bronchoscopy and CT scans are used to determine the degree of your TBM.
We also need to determine whether the severe TBM is actually the cause of the symptoms, because sometimes patients have multiple diseases and we would not want to assume that the TBM is the reason for your symptoms. We will check for significant acid reflux, voice box problems, evidence of immune problems and other lung problems, for example.
Why place a stent? Can I keep the stent in if it works?
The stent is a hollow tube made out of metal or silicone and it placed in the airway to keep it propped open. If the stent leads to significant relief of symptoms in patients with TBM, then there is a good chance that the TBM was in fact the cause of the symptoms. Also, the response to stenting it is a good indicator of whether surgery might work. Unfortunately stents are not good long term solutions because they almost always lead to complications if they are left in for more than a couple weeks.
Why do I have this disease? What exactly is it?
TBM is an uncommon condition characterized by the weakening of the tracheal and bronchial airway walls. This leads to collapse or narrowing of the airway. Nobody really knows how the diffuse adult form of this disease is caused. Some theories include chronic inflammation from reflux or other irritants, but at this time it is not clear.
Does everyone with tracheobronchomalacia need surgery?
Definitely not. Some patients are not well enough to tolerate surgery. Others do not have severe enough disease to warrant a major surgery. Still others have associated conditions which, if treated, might lead relieve symptoms. For example, weight loss, treatment of asthma, control of acid reflux, or even just a well-structured exercise plan might help enough to control symptoms.
In some patients who have severe TBM but do not undergo major airway surgery,symptoms are managed with medication, flutter valves to free up phlegm, continuous positive airway pressure (CPAP) to keep the airways open, or even tracheostomy tube placement.
Surgery for TBM
How is it performed?
During an open approach tracheobronchoplasty, your surgeons will create a standard posterolateral thoracotomy incision roughly 8-10 inches on your side, curving back behind your shoulder blade. We then go between the ribs to get into the chest. Sometimes we will need to cut a small piece of rib out to gain more space. We free up the windpipe and then place a plastic mesh into place to act as a support (splint). This takes 60-80 sutures to tack it into place.
With the robotic approach, several small incisions are made on your side and along your back under your shoulder blade. Instruments and cameras are inserted through these incisions and used by the surgeon to suture sections of mesh to create the splint for the floppy airway.
Many factors are evaluated to determine what approach would be the most appropriate. During your consultations with the thoracic surgeon, this will be discussed and decided prior to scheduling the surgery.
How long does it take?
Tracheobronchoplasty takes about 8 hours.
When I wake up from surgery will I have tubes in me?
There usually will be an epidural catheter, which delivers pain medication directly into your back, a bladder catheter, IVs and arterial line directly into veins and artery, and a drainage tube in the chest. You generally will not go home with any of these.
Will I have a breathing tube in when I wake up?
Usually the anesthesiologist will be able to remove the breathing tube at the end of the operation. Occasionally we will leave it in overnight or longer if necessary, but this is the exception to the rule.
Will I feel better right away?
Usually patients can tell that the air is moving better nearly immediately. However, there can be a lot of swelling of the airway and also phlegm (mucus) production that result from the surgical trauma. At the same time, because of discomfort from the large incision, it can be difficult to cough. This makes the first few days after surgery less strikingly better than it eventually should get.
Is it very painful? How will my pain be managed?
This incision (called a thoracotomy) can be painful so we will manage your pain with a combination of medications, including narcotics (‘pain meds’). Usually patients will need to take some pain pills for 2-4 weeks once they go home.
Will my body reject the mesh?
The mesh is made out of polypropylene and has been used for a long time to repair hernias. It is very safe, and while any foreign material in the body can get infected, there haven’t been any major issues. The mesh does not cause an allergic response.
Nevertheless, tracheobronchoplasty is a rare surgery worldwide,so long-term follow-up studies with thousands of patients are really not possible. We at BIDMC have the largest experience doing this surgery and have only had a few patients who have had problems with the mesh over a ten year period. It is important to know that while we think that over time the mesh should become very stably incorporated into the airway, we don’t have data to say what it will do over 20, 30 or 40 or more years after implantation. Obviously the things that the mesh could damage nearby are very sensitive structures such as lung, vessels, esophagus, or airway. Unanticipated problems with any medical implant are well-documented phenomena, and this a risk that you will discuss with your surgeon.
What are the other risks of surgery?
The primary risks are problems with breathing and infections. The risks of needing a breathing tube, supplemental oxygen, or even a tracheostomy tube for longer term management on a breathing machine depend a lot on your lung health before surgery, though any major, extensive operation in the chest can give these risks. In our experience only a small number of patients do need to get a tracheostomy for example. Pneumonia or tracheobronchitis does not affect the majority of patients, but those who have recurrent infections prior to surgery might be more likely to develop these conditions after surgery. Any major operation can give risks of bleeding, reoperation, organ dysfunction, poor wound healing, heart issues, stroke, clot, or other complications, but these are not overly common after this surgery. The risk of dying after this operation is low — around 1-2%. We will be working closely near the airway, lungs, esophagus, vessels, heart, nerves, and other structures in the chest so any of these could get injured inadvertently — however this is not a likely event.
What do I need to bring to the hospital?
You do not need to bring anything with you to the hospital. Please leave valuables at home or at your hotel. There is no need to bring your own medications to the hospital. Basic toiletries are provided during your stay.
What if I don't do the surgery?
Your symptoms may stay the same or worsen. However, it is unlikely that the symptoms or TBM will disappear. Unlike cancer, TBM is not a malignant disease and so your sense of how badly it may be impacting your quality, as opposed to length, of life is the most important factor to consider when thinking about surgery.
Recovery After TBM Surgery
How long am I in the hospital?
Usually patients are in the intensive care unit (ICU) 2-3 days and then another 5 days in a regular hospital unit.
Can someone stay with me while I'm in the hospital?
If absolutely necessary, a family member may sleep in the recliner next to the patient's bed if you are in a private room.
I am from out of town. How long will I have to remain local while recovering?
Patients need to remain in the local area for 2 weeks after discharge from the hospital.
How long am I out of work?
Usually 6-8 weeks. If the job has a lot of physical requirement it could be 3-4 weeks more.
When will I see the doctor after discharge from the hospital?
You will have a postoperative visit scheduled 2 weeks after discharge.
What happens if I have a problem after I get discharged?
Patients should call the thoracic surgery office at 617-632-8252 if they have any postoperative concerns. If there is anything life-threatening then call 911.
How long before I can drive after surgery?
Most patients will be cleared to drive by 2-4 weeks after surgery.
How long before I'm fully recovered?
Even though you should be back to most activities by 8 weeks, patients really might take 6-12 months to get over the nagging fatigue, aches and pains, incision sensitivity, and reconditioning.
TBM Surgery Outcomes
Does everyone get better?
About 80 percent of patients with severe TBM who respond well to a stent trial will get relief with surgery. Some patients do not. This is because of three potential reasons: 1) they have other medical problems which prevent symptom relief or make recuperation from surgery complicated, 2) the TBM progresses into areas beyond the areas that are able to be surgically repaired through the chest or it comes back in the areas that were repaired, and/or 3) there were technical limitations to the degree of re-shaping that was feasible with the surgery.
Is possible that that it could come back?
Some patients will have recurrence of TBM as their airways remodel what was a very anatomically-corrected airway after surgery. It is hard to know why, but in those rare patients we think that whatever was the underlying cause of the malacia in the first place continues to cause remodeling in the airways and basically undoes the stability of the mesh splint. Also in a minority of patients there is a progression of the TBM, either up into the short segment of trachea in the neck (above the repair that was done in the chest) or into the smaller windpipes that branch out into the lobes of the lung. Rarely we will do surgery on the neck to correct collapse there that developed after the main chest operation.
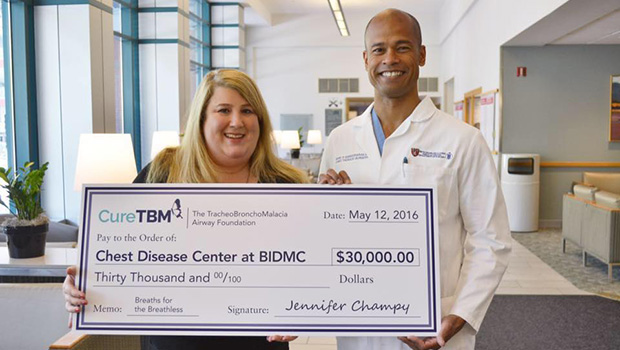
Setting Out to Cure TBM
A BIDMC patient’s ‘Cure TBM’ foundation raises funds and awareness of a rare lung condition treated by BIDMC experts.
Read the Full Article
Treating TBM: BIDMC Surgeons Provide Rare Expertise for Chronic Lung Condition
Sandra Rocha’s chronic cough lasted for decades before a diagnosis at BIDMC led to her life-changing treatment.
Read the Full Article
