What to Expect During Sarcoma Treatment
If you have been diagnosed with, or your doctor suspects, bone or soft tissue sarcoma, what can you expect at BIDMC? We work together with your referring physician to provide initial diagnosis and treatment, second opinions and/or long-term surveillance (follow-up care). We believe in open communication, personal attention and shared decision-making. We offer:
- State-of-the-art diagnosis and treatment, including clinical trials
- Multidisciplinary evaluation and treatment that gathers a team of experienced and compassionate physicians, nurses and other healthcare professionals working on your behalf
- Patient-focused and customized care, to respect your personal preferences and wishes
Our doctors, nurses and other healthcare professionals at BIDMC will help you learn about:
- Your cancer diagnosis, the tests you will have, and any necessary preparations
- The procedure or operation you will need
- Your recovery period, medications, returning home and much more
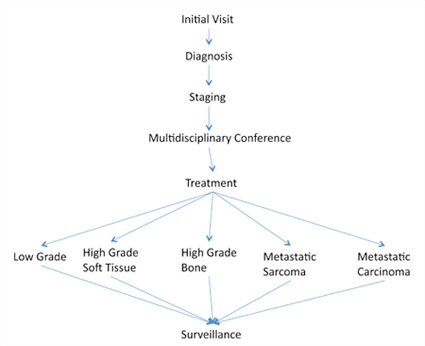
You can think about your care for sarcoma at BIDMC in terms of six general categories: your initial visit, diagnosis, staging, multidisciplinary conference, treatment and surveillance.
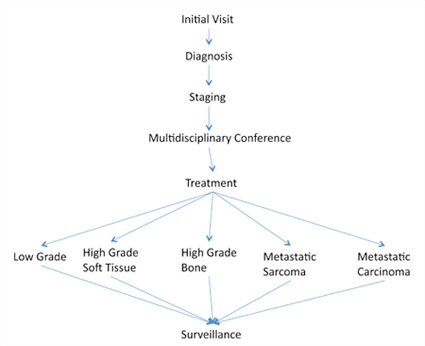
Initial Visit
Your initial visit involves physician evaluation, a review of any existing imaging studies that you might have (X-rays, MRI, CT scan and reports of these studies), and determination of next steps. If you have had a biopsy, it is important for us to review the report and have our pathologists look at the actual slides from the biopsy.
Diagnosis
We may need to do additional imaging (X-ray, MRI, MRI angiogram, CT scan) to find out more about the tumor and the area where it developed. Making a correct diagnosis also involves taking a biopsy - either by needle or surgical incision.
In an image-guided needle biopsy, musculoskeletal radiology physicians, guided by CT or ultrasound, insert a needle into the tumor to take a small core sample of cells for analysis. A surgeon is also present to help guide the needle's path. This outpatient procedure uses a local anesthetic to numb the area.
In an open biopsy, a surgeon uses a scalpel (surgical knife) to make a small incision and take a wedge of tumor for analysis. This is usually an outpatient procedure, but performed in the operating room with general anesthesia, so you are asleep.
Usually biopsy procedures are not carried out at the initial visit, but arranged for at a later date once all the information and imaging studies have been gathered.
Staging
Staging is the next step, to determine whether the tumor has spread and if so, where. More imaging studies may be necessary (CT, bone scan and PET scan). A surgical oncologist may also need to do an outpatient procedure called a sentinel node biopsy. Tumors with a tendency to involve lymph nodes require this type of biopsy. The surgical oncologist injects an area of the tumor with "dye," which is picked up in the lymph nodes. The lymph node(s) that are both the first to absorb the dye and absorb the largest amount are removed and examined to determine if they contain any tumor cells. (If so, the surgeon will remove these lymph nodes during the same or subsequent operation to remove the tumor, to be sure all traces of cancer are gone.)
Multidisciplinary Conference
At our weekly multidisciplinary conference, we review all of your information and combined recommendations for care. Our musculoskeletal radiologists report on your imaging studies and our musculoskeletal pathologists review the results of your tissue biopsy. Oncology surgeons (orthopedic and general), medical oncologists and radiation oncologists voice their opinions. Together as a team - focused solely on you - we reach agreement on the best treatment options for your particular sarcoma.
Sarcoma Treatment
The type of treatment we recommend is based on whether the sarcoma is low or high grade (low-grade tumors grow more slowly with a more favorable outlook), and whether the tumor is localized or metastasized. A localized tumor is confined to one area and more easily treated. Cancer that has metastasized has spread to other tissue or areas, which requires more aggressive treatment.
Low Grade Bone and Soft Tissue Sarcomas
Surgeons remove (or excise) the tumor. Our orthopedic oncology team of experts is internationally recognized for expertise in limb-salvage reconstructive surgery when removing the tumor to avoid amputation, preserve appearance, and promote the greatest degree of mobility. Limb preservation is based on your age and health, and tumor size and location. In limb-sparing surgery, once the tumor is removed, surgeons reconstruct any bone defects with bone graft, bone cement and/or metal replacements. They reconstruct any tissue defects usually with local tissue. Revolutionary advances in limb-sparing surgery and in limb prostheses if amputation is the best course of treatment, help preserve mobility and function, and sustain a quality of life that was until now not often possible.
Localized High Grade Soft Tissue Sarcoma
Radiation is the first treatment course if you have a localized (confined) high-grade (more advanced) soft tissue sarcoma. In some cases, you may need low-dose chemotherapy at the same time, in order to shrink the tumor before surgeons can remove it. Most often, following radiation and chemotherapy, surgeons can perform limb-sparing surgery to remove the tumor. Orthopedic oncology surgeons reconstruct soft tissue defects with local tissue, or with muscle flaps, with help from a plastic surgeon. If the tumor is very large, and sitting next to a nerve or blood vessel, for instance, it may be necessary to follow surgery with a boost of radiation from CyberKnife, to remove any traces of cancerous tissue. CyberKnife is precisely targeted radiation therapy, focused on the residual cancer cells, with minimal exposure to surrounding healthy tissue. You may also need physical therapy and rehabilitation to restore range of motion and function to the affected limb.
Localized High Grade Bone Sarcoma
If you have a localized (confined) high-grade (more aggressive) bone sarcoma, your treatment course is likely to include:
- Chemotherapy before surgery
- Limb-sparing surgery with metal bone and joint replacements, and allografts (donated bone graft), and reconstruction of soft tissue defects that may require muscle flaps, with assistance from a plastic surgeon
- Additional chemotherapy after surgery, which may be the same or different from the chemotherapy you received before surgery
- Physical therapy to restore range of motion and function to the affected limb
Metastatic Sarcoma
Metastases are cancer cells that have spread from an original or primary site to one or more locations or organs elsewhere in the body. Metastatic sarcoma means your cancer has spread from a primary site (such as the tumor in your arm or leg) to another area, usually the lung or lymph notes. If you are diagnosed with metastatic sarcoma, you will likely receive some combination of chemotherapy, radiation, and surgery, depending on the tumor and the areas of involvement.
Metastatic Carcinoma to Bone
Bone is the most common site of metastasis from cancer of the breast, prostate and lung. If you are diagnosed with metastatic carcinoma to the bone, physicians will assess your risk of fracture and if that is high, may recommend prophylactic (preventive) fixation of the bone with rods or plates and screws. Treatment is also likely to include:
- Radiation
- Chemotherapy and hormone therapy
- Interaction with other cancer care teams to treat your primary cancer
- Rehabilitation to improve function
Surveillance
Surveillance or follow-up care, after initial treatment for sarcoma, includes vigilant and regular self-exams, physician evaluation to address any symptoms, and radiologic scans to evaluate tumor relapse in the original site or in metastatic (spreading to) sites. Surveillance care continues at regular intervals for many years.