Bone Marrow Transplant FAQs
Frequently Asked Questions About Bone Marrow Transplant (Stem Cell Transplant)
The more correct term to use, instead of bone marrow, is hematopoietic progenitor stem cells, and to keep that simple, we'll use the phrase "stem cells."
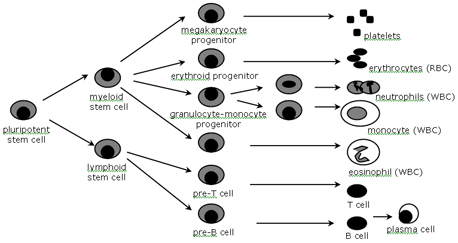
Stem cells, also referred to as pluripotent stem cells, are immature blood cells that can develop into red blood cells, white blood cells, and platelets. These blood cells are essential to life: red blood cells carry oxygen from your lungs to the rest of your body, including all your organs, and return carbon dioxide to the lungs to be exhaled; white blood cells prevent and fight infections; and platelets help the blood clot and prevent excessive bleeding. Stem cells are mainly concentrated in your bone marrow space in bones like the hips, sternum and skull. However, stem cells can also be found in the blood that circulates throughout your body (peripheral blood).
Stem Cell Maturation
Your bone marrow produces the pluripotent stem cells that are the basic blood forming cells. These stem cells mature into either myeloid or lymphoid stem cells. Myeloid stem cells then further develop into neutrophils, monocytes, and eosinophils (types of white blood cells), as well as red blood cells and platelets. Lymphoid stem cells divide into either T-cells or B-cells, which are important participants in the body's immune response to foreign matter.
So, with that basic information out of the way, let's go back to your original question: What is a stem cell transplant? A stem cell transplant is an intravenous transfusion that replaces damaged stem cells with healthy stem cells. These healthy stem cells then reproduce into red blood cells, white blood cells and platelets. The purpose of a stem cell transplant is to replace a patient's damaged bone marrow. Damage to bone marrow can occur because of disease (for example, leukemia) or because of high doses of chemotherapy that are given to treat cancer.
There are two main different types of stem cell transplants: autologous and allogeneic, and there are several types of allogeneic transplants.
Autologous Transplants
Autologous transplants utilize a patient's own stem cells. Prior to transplant, chemotherapy is given in doses much higher than standard regimens with the goal of maximizing tumor death. The primary problem with higher doses of chemotherapy is the complication of irreversible damage to the human bone marrow. In order to prevent this risk, stem cells are collected (another term used is harvested), frozen, stored, and then given back after completing high-dose chemotherapy. This is called a "stem cell rescue." The stem cells will repopulate the marrow space and, in approximately 10-12 days, will begin to produce white blood cells, platelets and red blood cells.
Allogeneic Transplants
Allogeneic transplants utilize someone else's stem cells. The donor may or may not be related to the patient.
There are three types of allogeneic transplants: ablative, reduced intensity (also called a mini-transplant, or non-ablative), and umbilical cord.
- Ablative Transplant (also known as "full dose" or "standard" allogeneic transplant) : The patient undergoes several days of high-dose chemotherapy and possibly radiation. This is known as the conditioning regimen. Other terms you might hear used are: transplant regimen, treatment protocol, or preparative regimen. The donor stem cells are then infused into the patient.
It is important to understand that how much chemotherapy you can give to treat a patient's disease is carefully regulated due to the damage chemotherapy can do to the bone marrow. Without a functioning bone marrow, a patient will not survive. In an ablative transplant, because the patient will be getting a "new" bone marrow, we can give much higher doses of chemotherapy because we do not need to worry about damage done to the bone marrow. Because of this, the hope and purpose of the higher doses of chemotherapy is to destroy any remaining diseased cells - Reduced Intensity (also known as non-myeloablative or "mini" transplants) :Lower doses of chemotherapy and possibly radiation are used as the conditioning regimen, followed by the infusion of donor stem cells.
Compared to an ablative transplant, the goal of this type of transplant is to use the donor's bone marrow to help fight the disease, as opposed to high doses of chemotherapy. This process is called many different names, but the main terms are graft-versus-tumor effect, or graft-versus-malignancy effect. The lower doses of chemotherapy and radiation suppress the patient's bone marrow (immunosuppression) just enough so the new marrow from the donor can start growing. If immunosuppression didn't happen, the patient's marrow would reject the new marrow and it wouldn't engraft, or start growing to create a new bone marrow. Once it starts to grow and flourish, the plan is that the newly functioning marrow and immune system will be more effective at killing the disease than the patient's own immune system was.
Due to the lower doses of chemotherapy and radiation, this type of transplant can be given to people who might not have been able to have an ablative transplant due to other health issues or age.
The term "mini" transplant, however, is somewhat misleading. Although patients receive less toxic dosages of chemotherapy and radiation, and may feel well early in the post transplant process, they are still at risk to develop serious and potentially life-threatening side effects. These side effects often begin 30-60 days post-transplant when the new immune system is gaining strength. - Cord Transplant: A third type of allogeneic transplant is an umbilical cord transplant. Sometimes we are unable to find an adult donor for a patient. In those circumstances, we can almost always use donated cords. The umbilical cord from a newborn baby is rich with stem cells. After a delivery, if someone so chooses to donate, these cords are typed, and then they are put in a cord blood bank, waiting for a patient match.
Stem cells used in the transplant can come from three sources in the body:
- Blood - Remember that there are a certain number of peripheral stem cells circulating in the blood. To collect these cells for transplant, medications can be given to "push" more of these stem cells from your marrow into the blood. The blood can then be collected through a process known as apheresis, and the stem cells can be separated out, removed or harvested (all terms for the same process) for the transplant.
- Bone marrow - In some cases, the stem cells are removed directly from the bone marrow through a surgical procedure.
- Umbilical cord - The umbilical cord from a newborn baby is rich with stem cells. These cords are sometimes used as a source of stem cells.
During your transplant, the number of blood cells (WBCs, RBCs, and PLTs) in your body will drop. To monitor this effect, we will be watching your "blood counts" very closely. Important decisions about your care will be made according to the results. For several weeks, a "complete blood count" or CBC will be drawn daily. The CBC gives information about the level of WBCs (white blood cells), RBCs (red blood cells), and PLTs (platelets) in your blood.
The normal WBC is anywhere between 4,000 and 10,000. When your WBCs fall below 1,000 you will be at greater risk for infection. A low level of WBCs is called neutropenia. There are several different types of white blood cells. One type you may hear about is the neutrophil. Neutrophils are very important for fighting infection and are often counted separately. When the neutrophil count is less than 1,000, you are at a higher risk for infection. You may hear clinicians use other names for the neutrophil, such as "polys" or granulocyte." You may also hear them talking about the "ANC" which refers to the "absolute neutrophil count," or the "TGC" - the total granulocyte count. These tests give your team information about how well your body is able to respond to bacterial infection.
RBCs are measured by values called hemoglobin (Hgb) and hematocrit (Hct). The normal Hgb is anywhere between 14 and 18, and a normal Hct is between 37 and 52. When your RBC count is low, which is an expected side effect of the treatment you will be getting, these values will fall. This is a condition called anemia. If you develop anemia, you will likely feel more tired and/or short of breath than usual.
A normal platelet count is between 150,000 to 400,000. When this value falls below 50,000, something that is very common, you will be at greater risk for bleeding. This is a condition called thrombocytopenia.
 You will have a private room with a private bathroom, cupboard and closet, small refrigerator, TV, DVD/VCR player, Internet connection, I pod doc, and a radio/CD/cassette player. Hospital gown, robe and pants will be provided, though you may choose to bring more clothing (see below).
You will have a private room with a private bathroom, cupboard and closet, small refrigerator, TV, DVD/VCR player, Internet connection, I pod doc, and a radio/CD/cassette player. Hospital gown, robe and pants will be provided, though you may choose to bring more clothing (see below).
Suggested Items to Bring
- Comfortable clothing:
- Must be washed, dried in a dryer and immediately placed in a tied or zip-locked plastic bag. This applies to new or old clothing.
- The clothing you wear to the hospital and other stray clothing will NOT be allowed into the transplant room.
- Shirts should be button down or have a wide neck for easy access to your central line catheter.
- While in transplant, your caregiver can continue to do laundry for you, following the guidelines above - New, loose slippers/Crocs/sandals (with traction on the bottom) to protect feet
- DVDs or VHS tapes
- Music
- Personal laptop computer (although laptops are available to borrow) and web cam
- Books or magazines
- Games or puzzles
- Journal or writing paper
- Photos of your family and friends; posters and wall décor that can be taken down
- Electric razor (for men who plan to shave)
- Hard candy such as Jolly Ranchers
- Soft toilet paper, flushable toilet wipes, soft tissues (that may be softer than hospital brand)
- Food
- Beverages must be in individual containers and snacks such as cookies or crackers must be in single serving packages (for example: no bags of chips or boxes of cookies). Must be "one time use" packaging.
- Cooked food should be prepared according to the guidelines outlined in the "Nutrition" section of the educational guide you receive. Cooked food must be placed in individual servings and immediately frozen after being prepared. Commercial frozen dinners are permitted. - Pillow (optional): must be brand new and still in its original packing
- Personal blanket/throw (optional): must be brand new and still in its original packing
Do Not Bring
- Plants or flowers
- Toiletries such as deodorant, shaving cream, make-up, scented soaps or lotions
- Your own medications, vitamins, herbs or supplements
- Dental floss or toothbrush
- Standard razor
Visitors are encouraged throughout your hospital stay, and are welcome. Visitors often provide a needed break in the daily routine. Although the Bone Marrow Transplant Unit does not have strict visiting hours, suggested visiting hours are between 11 a.m. - 9 p.m., so that you can get proper rest. There is flexibility to these suggested times, but no one is allowed to stay overnight in your room.
Visitor Guidelines
The guidelines below may seem like harsh rules to follow, but our goal is that your loved one/ friend moves through the transplant process with as little difficulty as possible. Part of that involves taking every effort to protect against infection. Please remember your loved one/ friend may be experiencing fatigue and side effects related to treatment. Ask your loved one/friend how long you should visit, and respect that time limit. If you have any questions or concerns regarding these guidelines, please feel free to ask anyone on our team.
- Absolutely no visiting if you are ill. Please check in with the nurse if you have had any recent vaccinations.
- Children under 6 years old are NOT allowed on the BMT unit. For those children 6 years of age or older, children must be screened by the nurse at the front desk prior to visiting. Child must wear a sticker (symbolizing that they were screened) at all times while on the unit.
- All of your loose personal belongings (coats, pocketbooks, etc.) must be kept outside of the room. Lockers are provided to store your personal items securely.
- Any items being brought to the patient must be checked with the nurse before being taken into the room. Absolutely no fresh flowers or plants!
- Before entering the room:
• Put on a mask if patient had an Allogeneic Transplant
• Wash your hands at sink or use Cal stat (waterless hand sanitizer) found in hallway
• Put on gloves
• Open the patient's door with your elbow - NOT with your GLOVED HANDS - Keep the door to the room closed at all times.
- While in the room:
• Always keep gloves on
• If patient had an Allogeneic Transplant, always keep a mask on
• Do not eat or drink in the room
• Do not use the patient's bathroom or telephone
• Limit physical contact with the patient
Where should we park? How much does parking cost?
The closest hospital garage to the unit is the Feldberg Garage, which is located at 330 Brookline Avenue. Discounted parking stickers are available for the main family member. Your transplant nurse or social worker can give you more information. Other visitors will pay the regular rate in the garage, although there is a discounted rate if the visit is over 2 hours.
Family and friends may bring in food items for you, but the nurse should check the items first. A refrigerator is available in your room. You will be given an educational guide, and anyone bringing you food or beverages should follow the guidelines in the "Nutrition" section of that guide.
Basic guidelines are:
- Beverages must be in individual containers, and snacks such as cookies or crackers also must be in single-serving packets. (For example, a box of cookies is not allowed.)
- Cooked foods should be prepared according to the guidelines in the "Nutrition" section, and then frozen in individual servings immediately after being prepared.
- Food items in the room are for the patient only. Family and friends may not share food once it has been brought into the room.
